Booster shots are crucial to preventing serious illness and death as people’s immunity — both from vaccines and previous COVID-19 infections — wanes, the Omicron variant sweeps the country and Ohio’s hospitalizations soar, health experts said.
Recent studies have shown that boosters of mRNA vaccines from Pfizer and Moderna significantly increase protection against the highly transmissible Omicron variant now causing the majority of cases in the U.S.
Readers continue to have questions about booster shots, how they work, why we need them and which one is best for them. So the Dayton Daily News asked a local virologist, an epidemiologist and a pharmacist to answer those questions.
Experts quoted in this article are:
- Dawn Wooley, Wright State University professor with a doctorate in virology
- Timothy N. Crawford, Wright State University professor with a doctorate in biostatistics and epidemiology
- Zach Jenkins, clinical pharmacist with Premier Health and professor of pharmacy practice at Cedarville University
After previously only recommending boosters for the elderly and most vulnerable, the Centers for Disease Control and Prevention now encourages all Americans 16 and older to get their booster shot. Adults should get a booster shot from any approved manufacturer if it’s been at least six months since completing the vaccine series for Pfizer or Moderna or at least two months since getting a Johnson & Johnson shot. Only Pfizer boosters are authorized for 16- and 17-year-olds.
About 41% of Ohioans have not gotten any coronavirus vaccine doses. They will bear the brunt of the omicron wave (about 85% of COVID-19 patients in Dayton-area hospitals are unvaccinated). But the millions of Ohioans who are vaccinated but not boosted could also have a rough time during this winter surge.
About 21% of Ohioans have received their initial vaccine series plus an additional dose. This leaves about 39%, over 4 million Ohioans, somewhere in the middle, with many of them eligible for a booster.
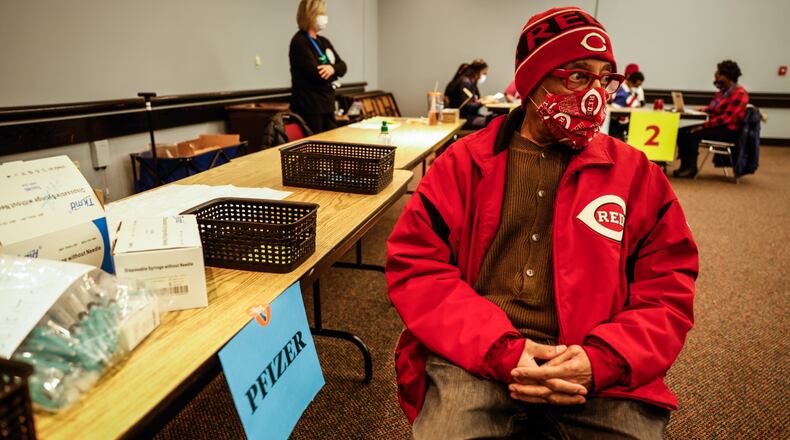
Steven Phillips, 73, from Dayton, received a COVID-19 booster shot at the Dayton Convention Center in early December. He wishes more people would get the recommended shots.
“I can’t understand why it’s not more, why people are so hesitant when people are dying from (COVID-19) and the after effects,” he said.
Here’s answers to readers’ questions about boosters.
Q: Why do we need COVID-19 booster shots?
Wooley: Studies have shown that levels of protective antibodies decline significantly at approximately six months after the second shot, so the booster is recommended at this time.
Crawford: Although vaccine effectiveness remains high for preventing severe disease and hospitalization, we are seeing that protection from infection or mild symptoms is waning. In other words, the effectiveness of the vaccine to prevent infection is decreasing with variants like Delta and Omicron. The booster shots are needed to provide an added level of protection, especially among those 65 years of age and older. The boosters essentially increases the immune response, which in turn increases protection against infection.
Q: How do booster shots work?
Wooley: Boosters remind our immune system about what the virus looks like. In response, our immune system ramps up production of circulating, protective antibodies so that they are ready to act immediately upon infection.
Jenkins: Booster shots work by stimulating your immune system with re-exposure to a viral particle. In this case, the particle is the spike protein from the SARS-CoV-2 virus. Once stimulated, your immune system produces antibodies and increases expression of t-cells, beta-cells, and other intermediaries involved with both short-term and long-term immunity. The good news is that a booster can help people who have been previously exposed who may not have developed a complete immune response.
Q: Who should get a booster shot?
Crawford: The current recommendation is that if it has been at least six months since completing the vaccine series for Pfizer or Moderna, or at least two months for Johnson & Johnson, adults aged 18 years of age and older should get a booster shot. For Pfizer, this also includes 16-17 years old.
Wooley: Anyone who is eligible should get the booster. Keep in mind that a relatively small number of people have had an allergic reaction to the first or second shot and should not be boosted. Also, some people have other medical conditions that contraindicate being vaccinated at all. For these reasons, those who are healthy enough to be vaccinated should do so to protect the vulnerable population who cannot be vaccinated.
Q: Previously, only older people and people with medical conditions were advised to get a booster shot. Why has the advice changed?
Jenkins: There are three main reasons:
1. We have multiple viral strains in circulation that are more equipped to evade your immunity from previous infection or immunization. This means that you stand a higher likelihood of being infected and transmitting infection to others.
2. Omicron is of a different lineage from all other viral strains to date. This means that previous immunity will likely be less protective against infection, although we need more data to truly know if this is the case. The current evidence would suggest that boosting will generate increased protection against Omicron in the short-term, albeit this protection will likely be less helpful than developing an updated vaccine to account for new variants (this takes time to do).
3. The benefits of short-term immunity from previous infection or immunization have faded over time, and more and more people are experiencing symptomatic illness. In some cases, this has resulted in individuals making trips to the emergency department or being hospitalized with COVID-19. However, long-term protection against severe disease (the kind to land you in the ICU or kill you) has held up.
Q: Will this booster shot protect me from Omicron? What about future variants?
Wooley: Early indications show that the current vaccine may not be as effective against the Omicron variant as it was against the Delta variant. However, the Omicron variant appears to be less virulent (harmful). The trend in viral epidemiology is that the virus becomes more transmissible but less pathogenic (causing less disease) at later times in the epidemic or pandemic. This phenomenon is due to the fact that as the first mutates to become more transmissible, there is a trade-off in function by which it becomes less pathogenic. From an evolutionary standpoint, it is disadvantageous for the virus to kill its host too quickly because it will run out of susceptible hosts and extinguish itself. Since the current booster is based on the original SARS-CoV-2 strain, it will also be less effective against Omicron as is the original vaccine.
Jenkins: It’s hard to predict what other variants may emerge. The virus can only mutate so many times without doing harm to itself and making itself less effective at spreading. With this in mind, we can’t say for certain if this will protect against all future variants. The current thought is that stimulating several parts of your immune system, such as t-cells, may help your immune system to pivot with exposure to new strains.
Crawford: Recently some preliminary data from Moderna suggests that the antibody levels against the Omicron variant is much higher for the booster shot compared to an individual with just the two dose series. So, that’s promising, but of course the data are preliminary.
Q: What kind of booster shot should I get? Can I mix and match manufacturers? Should I?
Crawford: You can mix and match as some studies have shown no major effects from mixing and matching manufacturers. However, the Centers for Disease Control and Prevention just endorsed a recommendation from the Advisory Committee on Immunization Practices for individuals to choose an mRNA vaccine (Moderna or Pfizer).
Jenkins: The data would suggest that mRNA boosters are the best for all individuals, regardless of which vaccine they received first. The Moderna vaccine seems to be holding up the best against new variants overall, but the Pfizer vaccine isn’t too far behind. There is also mounting evidence of an increased risk of myocarditis in young individuals (less than 40 years of age) who receive Moderna vs. Pfizer. A large U.K. study recently indicated that this risk may supersede the risk of myocarditis associated with SARs-CoV-2 itself. As such, I would personally encourage those under the age of 40 (men in particular) to choose Pfizer over Moderna. For those over 40 years of age, I think the choice matters less. In particular, I would encourage those who are at high risk of severe disease to consider Moderna over Pfizer. As with any of my recommendations, I would also suggest having a personal conversation with your medical provider.
Wooley: The J&J vaccine is currently under scrutiny again for causing blood clots, some of which are fatal. Therefore, it would be prudent to seek the mRNA type of vaccine (Pfizer or Moderna) at the current time. If someone has previously received the J&J vaccine, they may receive the mRNA vaccine as a booster. In fact, some preliminary studies show that receiving the mRNA booster after receiving the original J&J vaccine is leading to high levels of protective antibodies. However the opposite mix-and-match is not advised; if someone has received an original mRNA vaccine, they should stick with the mRNA vaccine for the booster.
About the Author